Hip Replacement Prosthesis: Types and Procedure
Hip Replacement Surgery
When is a Hip Replacement Necessary?
When the hip is damaged, the first approach is conservative treatment, which may include rehabilitation, physiotherapy, pain medication, or a combination thereof.
However, if the damage is extensive or chronic, hip replacement surgery should be seriously considered. Persistent pain and the inability to perform even the simplest daily activities often convince patients to opt for surgery.
Hip replacement is performed when the natural joint is no longer functional, offering three treatment options: total replacement (arthroplasty), replacing both the femoral and acetabular components; partial replacement (hemiarthroplasty), preserving the acetabulum while replacing the rest of the joint; and partial prosthesis, suitable for younger patients without osteoporosis, sparing the femoral neck while treating other parts of the joint.
How is Hip Replacement Surgery Performed?
Hip replacement surgery is usually performed under general anesthesia, but epidural anesthesia, where only the lower body is numb, is also possible. Patients opting for epidural anesthesia are still sedated with powerful sedatives.
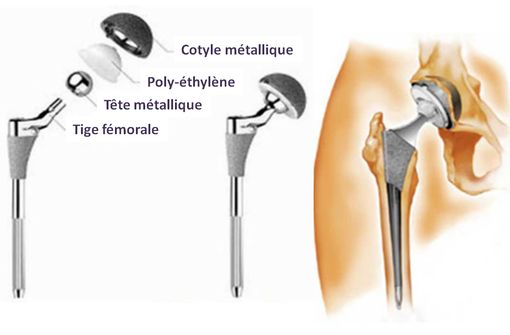
The procedure typically takes 60 to 90 minutes. The damaged upper part of the femur and the acetabular component are removed. An artificial metal alloy prosthesis is then inserted. The surgeon first attaches an artificial cavity to the pelvis, which acts as the acetabulum (a prosthetic cup). Next, a prosthetic stem is inserted, one end fused to the remaining femur, the other end featuring a head that fits inside the prosthetic cup.
The cup and stem head are secured using either acrylic cement or a press-fit mechanism.
Types of Hip Replacements
Total Hip Replacements
Total hip replacements are a crucial medical solution for restoring joint function in individuals whose natural joint has lost its effectiveness. This procedure, also known as arthroplasty, involves the complete replacement of both components of the joint: the femur and acetabulum. This surgery aims to improve mobility, relieve pain, and restore quality of life. Total hip replacements come in various designs, each tailored to specific needs, proving particularly beneficial for individuals suffering from various conditions affecting the hip joint. Utilizing advanced technologies and materials, these prostheses offer a durable and effective solution to improve functionality and restore well-being for those facing severe joint problems.
Partial Hip Replacements
Partial hip replacements offer a targeted approach to treating joint problems without total joint replacement. For example, a hemiarthroplasty preserves the acetabulum while replacing the rest of the joint, maintaining a portion of the natural structure. This is particularly suitable for certain cases, providing a less invasive solution for younger patients without osteoporosis. Another option is a partial prosthesis that spares the femoral neck while treating other parts. This approach is carefully selected to meet individual needs, improving mobility, reducing pain, and minimizing the impact on bone structure. Partial hip replacements play a crucial role in personalized orthopedic care, enhancing patient quality of life.
Choosing the Right Hip Replacement
Size of Hip Replacement
Several size options exist: resurfacing prostheses, precisely covering the bone surface without removal; mini-prostheses, small implants sparing the femoral medullary canal; and traditional prostheses (cemented or uncemented), occupying the upper proximal half of the operated femur.
The size of the new prosthetic femoral head is also crucial. The natural femoral head's width significantly contributes to hip stability. Replacement inevitably results in smaller head diameters, except with resurfacing.
Materials of Hip Replacements
Understanding the differences between prostheses requires considering the materials, as they bear the stress of movement.
This is paramount for long-term prosthesis survival. Prosthesis detachment and failure, in over 95% of cases, stem from interface wear and debris release. The body's inability to digest this debris disconnects the prosthesis, resorbs peri-prosthetic bone, leads to prosthesis mobilization, and ultimately requires revision surgery. Each bearing pair has strengths and weaknesses. Metal-on-metal, used in resurfacing, has shown high failure rates and metallosis, complicating revision surgery. Metal-on-metal prostheses are now largely abandoned. The latest generation of cross-linked polyethylene, combined with 36mm ceramic or metal heads, show near-zero wear and failure rates after over 14 years of clinical data.
GET A QUOTE
Need more information?
Your health, our priority.
Request your free quote
The Surgeon's Choice
Over 60 hip replacement designs exist, but fewer than ten are commonly used.
The surgeon chooses the most suitable prosthesis considering:
- Patient's age;
- Body weight and material fragility;
- Potential allergies to prosthesis materials;
- Patient's sex;
- Underlying pathologies;
Patient age is critical. Older patients may not need the most durable or uncemented prosthesis, as a second replacement surgery is less likely. Younger patients need durable, potentially uncemented prostheses, delaying replacement and simplifying future procedures.
Hip Replacement Recovery Time
Patients can begin walking with precautions and crutches immediately post-surgery if conditions allow.
With regular, non-excessive rehabilitation, normal activities can resume within 2-3 months.
Avoid sudden movements and impacts; contact sports like football, skiing, and horse riding should be avoided. Driving can resume after about 6 weeks, work after 6-12 weeks depending on the profession, and sexual activity after 6-8 weeks with doctor's approval.