How is a cornea transplant performed?
Preparing for the procedure
If you have a corneal abnormality that causes visual impairment, ophthalmologists may recommend a cornea transplant.
A few days before the surgery, a general medical examination and routine laboratory tests (such as blood tests and an ECG) are performed to ensure that you are fit for surgery. You should not take aspirin for two weeks before surgery as it tends to cause bleeding. You will usually use antibiotic drops one day before surgery to protect the eye from infection. Do not eat or drink anything after midnight before surgery (ask your doctor to prescribe medication on the day of surgery).
The procedure itself
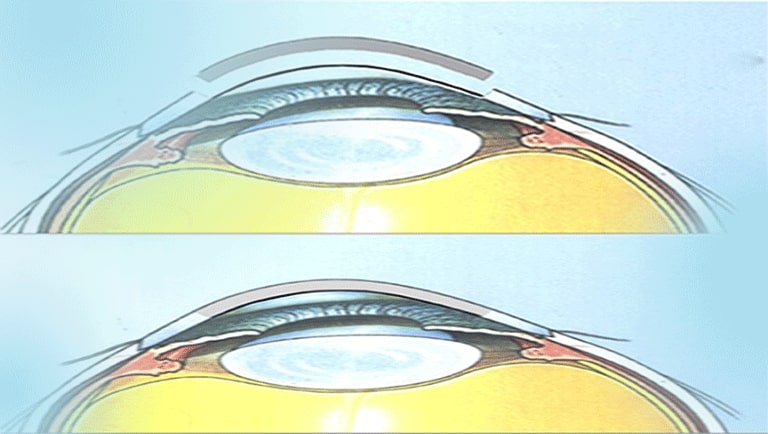
Not so long ago, if a failing cornea needed a transplant, a penetrating keratoplasty, i.e. the replacement of all layers, was used in 100% of cases.
New techniques allow for the transplantation of only the layers of tissue affected by the various corneal pathologies.
Today, it is possible to limit the replacement to only the endothelial layer (the very thin inner layer that regulates the hydration of the cornea and maintains its transparency), or a more or less superficial corneal layer.
In the first case, the advantage is that the mechanical structure of the cornea is left almost unchanged, avoiding the generation of high astigmatism, or points of increased fragility of the eye in the case of perforating corneal trauma.
In the second case, opacities of the superficial layers of the cornea can be removed, while preserving the patient's endothelium. Indeed, in some corneal diseases, this layer is in a healthier state than that of the donor.
Finally, by avoiding the replacement of the endothelial layer, the risk of developing rejection reactions is reduced.
Here are two of the main cornea transplant techniques frequently used today:
- Anterior Lamellar Keratoplasty ALK (Anterior Lamellar Keratoplasty). Indications for the procedure include superficial corneal scars, corneal opacities following refractive surgery, infections of various natures, dystrophies (particularly granular type) and corneal degenerations. In this type of surgery, a superficial corneal flap 130-160 µ (thousandths of a millimetre) thick is transplanted. The donor graft is usually cut to a thickness equivalent to that of the tissue removed from the recipient bed, and is sutured with simple radial 10-0 nylon stitches. The thickness of the recipient cornea is the main limiting factor. To avoid the risk of perforation, the lowest pachymetric value of the recipient cornea should not be less than 400 microns. The sutures are completely removed within 6 months of the operation, and visual recovery is faster than with penetrating keratoplasty. Postoperative astigmatism values do not differ significantly from those found after PK and patients can be corrected with glasses or contact lenses in a similar percentage of cases. Scarring only occurs in a peripheral annular zone of the cornea, while the recipient and donor layers are free to face each other in a large central area. This creates a more stable scar than with penetrating grafts and the eye heals faster and with less astigmatism than with penetrating operations. The surgery restores the normal anatomy of the cornea by providing a new Bowman's membrane and there is no significant scar formation in the optical zone after surgery. In addition, if necessary, it allows for new excimer laser treatments for refractive purposes;
- DSEK (Descemet's Stripping Endothelial Keratoplasty). A graft of stroma and endothelium from the donor is transplanted onto the inner surface of the cornea. The recipient corneal endothelium is removed, using a Sinsky hook and forceps, under viscoelastic protection. An abrasive spatula is used to create an adhesive surface in the recipient along the margin of the removed endothelium area. Manual dissection of a lamella of stroma and donor endothelium is performed. A disc of the desired size of endothelium-stroma is precisely cut out using the punch. The viscoelastic layer is completely removed from the anterior chamber. The endothelial lamella is implanted, introduced using a metal gutter that folds it like a "taco" and allows it to pass through a 2.8 mm tunnel. The lamella is then glued by filling the anterior chamber with air;
GET A QUOTE
For more information
Your health, our priority.
Request your free quote
Post-cornea transplant treatment
Back home, the patient can resume their daily life, they can read, watch television, go out. The ophthalmologist primarily recommends avoiding any pressure on the eyeball and washing their hands thoroughly each time eye drops are instilled. Treatment consists of cortisone and antibiotic eye drops for about 6 months. The recovery period is usually one month. The return to work is subjective.
In the weeks immediately following the cornea transplant, it is necessary to avoid all actions likely to cause an increase in thoracic or abdominal pressure and, consequently, intraocular pressure (for example, lifting weights, straining during defecation).
Swimming in a pool is also inadvisable in the first few months due to irritation caused by disinfectants and the risk of contracting potentially very serious infections.
It is quite normal for vision to still be "hazy" one month after a cornea transplant: the transplanted cornea needs a few months to achieve perfect transparency and relaxation of the often present stromal folds.
In addition to corneal transparency, other factors can delay visual recovery: postoperative astigmatism and re-epithelialization of the ocular surface. All these elements should be discussed with your ophthalmologist.
In general, visual function should already reach a correct level 6 months after surgery, then gradually increase.