Corneal Transplant: For Whom, Why, and How?
Corneal Transplant: Why and For Whom?
The Goal of a Corneal Transplant
Today, ophthalmic surgery aims to be as minimally invasive as possible. This goal is perfectly achieved in the case of refractive surgery, for example, which uses cutting-edge instruments and technologies that eliminate the use of blades, scalpels, and stitches. Even in the case of a corneal transplant, the ophthalmologist strives, as far as possible, to operate only on the part affected by a disease and requiring a graft. The morphology of the cornea, due to its layered fiber structure, helps and facilitates the achievement of this objective. This is why we can now talk about corneal grafts in the plural, generally referring to two types of keratoplasty: lamellar and penetrating.
Lamellar keratoplasty is used when only a layer of the cornea needs to be replaced. The word lamellar comes from lamella, as only the diseased layers of the cornea are operated on, leaving the healthy layers intact. Anyone suffering from keratoconus at an early stage, with injuries or ulcers resulting from trauma or caused by eye diseases and therefore no longer having perfectly clear vision, now resorts to lamellar keratoplasty.
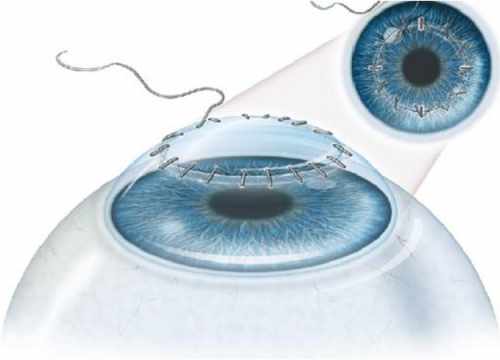
Penetrating keratoplasty, on the other hand, is a more invasive procedure, as it involves replacing the entire cornea, which has become opaque, not thick enough, or excessively curved due to a pathology (advanced keratoconus, for example) or trauma.
Indications for Corneal Transplantation
The cornea can undergo various alterations, such as trauma perforating the cornea, chronic infections, or changes in shape that reduce its transparency and consequently affect visual capacity. When this occurs, in many cases, the only possible solution is keratoplasty or a corneal transplant.
This leads to opacification of the cornea, and the patient begins to experience visual disturbances. Here are the cases in which the transparency of the cornea can be affected:
- Repeated infections such as keratitis, usually caused by bacteria or viruses, can cause ulcers in the cornea, so that the scar tissue that forms is somewhat more opaque than the original healthy cornea.
- Trauma or chemical burns can also make the cornea more opaque.
- Corneal dystrophies are a group of diseases that lead to a loss of corneal transparency without an inflammatory process. These are alterations that affect both eyes, generally appearing in the first decades of life and progressing slowly and gradually.
- Keratoconus is a progressive corneal degeneration in which the normal hemispherical structure of the cornea transforms into a cone due to thinning of the central area. It is usually bilateral but not symmetrical and makes vision increasingly blurry as it progresses.
- With age, the cornea, like any tissue, ages and can degenerate in various ways, forming a peripheral arc (arcus senilis) that does not affect visual capacity, or with diffuse involvement of grayish marbling that also generally does not affect vision, known as farinata cornea (flour-like cornea).
Procedure of a Corneal Transplant Operation
Corneal transplant surgery involves removing the diseased tissues from the patient and replacing them with healthy tissues taken from a deceased healthy donor. The transplanted tissue is then sutured to the periphery of the patient's cornea. Other surgical interventions, such as glaucoma or cataract surgery, can be performed at the same time. Corneal transplantation can be performed under local or general anesthesia.
The femtosecond laser represents the latest innovation in corneal surgery because it allows for extremely precise and regular cuts and incisions on the cornea, ensuring predictable and absolutely satisfactory postoperative results.
In diseases of the ocular surface, corneal transplantation may not be decisive. Indeed, in many cases, it is necessary to restore the integrity of the ocular surface first. This is now possible thanks to the use of amniotic membrane grafts on the ocular surface or by the reconstruction of healthy tissue from the stem cells of the corneal epithelium, contained in the limbus.
EXPRESS QUOTE
Would you like more information?
Votre santé, notre priorité.
Demandez votre devis gratuit
Corneal Transplant: What Complications and Outcomes?
In general, corneal transplantation has a good prognosis, as the risk of rejection is lower than for other organ transplants, the cornea being an avascular tissue.
In the case of lamellar corneal transplantation (partial replacement of corneal tissue), the risk of rejection is further reduced, as is the rate of secondary complications (e.g., hypertonia, infections), and visual recovery is faster.
The first postoperative check-up is performed the day after the operation.
Subsequent check-ups are initially weekly, then monthly.
It is essential that the patient after a corneal transplant carefully follows the prescribed treatment and continues their daily activities normally, respecting basic hygiene rules and avoiding excessive physical exertion.
The ophthalmologist will decide when to remove the suture based on the induced astigmatism and the time elapsed since surgery. However, the suture can only be completely removed 12 to 18 months after the operation.
Complete visual recovery can take several months, or even a year.
The patient should immediately consult their ophthalmologist in case of:
- reduced vision
- appearance of eye redness
- pain
If treated in time, most rejection reactions disappear with medical treatment.
[dt_sc_button title="Free Quote" size="medium" style="bordered" icon_type="" link="url:https%3A%2F%2F127.0.0.1%2Ftds%2Fdevis%2F" textcolor="#ffffff" bgcolor="#0c73ba"]