Corneal Graft: Procedure, Rejection Risks, and When it’s Necessary?
What is a Corneal Graft?
The cornea is a transparent membrane half a millimeter thick, composed of five superimposed cellular layers. It's the eye's first lens, through which light rays pass. Opacification or discoloration can cause serious visual impairment and lead to blindness.
A corneal graft, also called keratoplasty, is a surgical procedure that replaces part of the cornea with corneal tissue from a donor. The cornea is the transparent, dome-shaped surface of your eye where light enters, and it's crucial for clear vision. This surgery restores vision, corrects visual disorders, reduces pain, and improves the appearance of a failing or diseased cornea.
Corneas used in grafts come from deceased individuals. Unlike organs such as the liver and kidney, tissue compatibility isn't required for corneal grafts.
This surgical procedure has seen significant advancements in the last 10 to 15 years. Previously, it always involved replacing the entire corneal tissue. Now, it's selective tissue transplantation. Only the diseased part is removed, leaving other layers intact. This leads to faster visual recovery, fewer complications, and a minimally invasive procedure. We've moved from a full-thickness graft (penetrating keratoplasty, still necessary for damage at all levels) to a lamellar graft.
When is a Corneal Graft Necessary?
A corneal graft is necessary in several cases:
- Congenital diseases (present at birth);
- Trauma from accidents;
- Infections that cause corneal opacity or deformation, progressively impairing vision;
Corneal diseases often affect both eyes, causing near-total blindness (most common in 15-35 year olds). There's no age limit for corneal grafts; the operation can restore sight for both young and elderly individuals.
How is a Corneal Graft Performed?
Before surgery, specific examinations assess corneal health:
- Endothelial Microscopy: checks cell density, diagnosing degeneration and dystrophy of the corneal endothelium;
- Corneal Pachymetry: measures corneal thickness, assessing pathologies like keratoconus, corneal edema, and glaucoma;
- Corneal Topography: measures the curvature of the corneal surface;
- Pentacam: analyzes shape, anterior chamber depth, thickness, anterior surface elevation, and irido-corneal angle;
Surgery involves two steps:
- Excision of the recipient's diseased cornea using a corneal trephine and its removal;
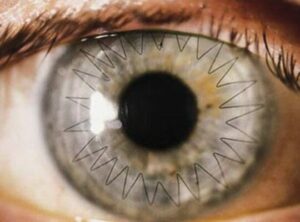
- Suturing the donor cornea into the recipient's eye using a very fine thread;
Cornea banks play a crucial role, collecting, analyzing, storing, preparing, and distributing corneas. Unsuitable corneas are used for eye disease research.
What are the Risks of a Corneal Graft?
Complications include rejection, trauma, infection, and refractive errors (like severe astigmatism).
Rejection is an immunological complication treated with immunosuppressant drugs and cortisone. It can be reversible, but sometimes a new transplant is necessary. Following the ophthalmologist's instructions is crucial.
EXPRESS QUOTE
Would you like more information?
Your health, our priority.
Request your free quote
What Precautions Should Be Taken After a Corneal Graft?
After a corneal graft, precautions ensure proper healing.
The patient should:
- Follow the prescribed treatment carefully;
- Resume daily activities normally, maintaining hygiene and avoiding excessive exertion;
The ophthalmologist determines suture removal based on astigmatism and time since surgery. Complete suture removal takes 12-18 months.
Full visual recovery takes several months to a year.
Immediately consult the ophthalmologist for:
- Decreased vision;
- Eye redness;
- Pain;
Most rejection reactions respond to prompt medical treatment.
What is the Success Rate of a Corneal Graft?
The success rate is very high (over 90% survival at 10 years), thanks to professional expertise, advancements in surgical procedures, and high-quality corneas.
Success rates exceed 90% for keratoconus, dystrophy, and corneal degeneration; around 80% for neovascularization and pseudo-keratoconus; and 60% for post-keratotic leucoma, corneal ulcer, or repeated grafts.